PA shouldn’t stand for
Pain in the Administration.
In its current state, medical prior auth is a burden on everyone.
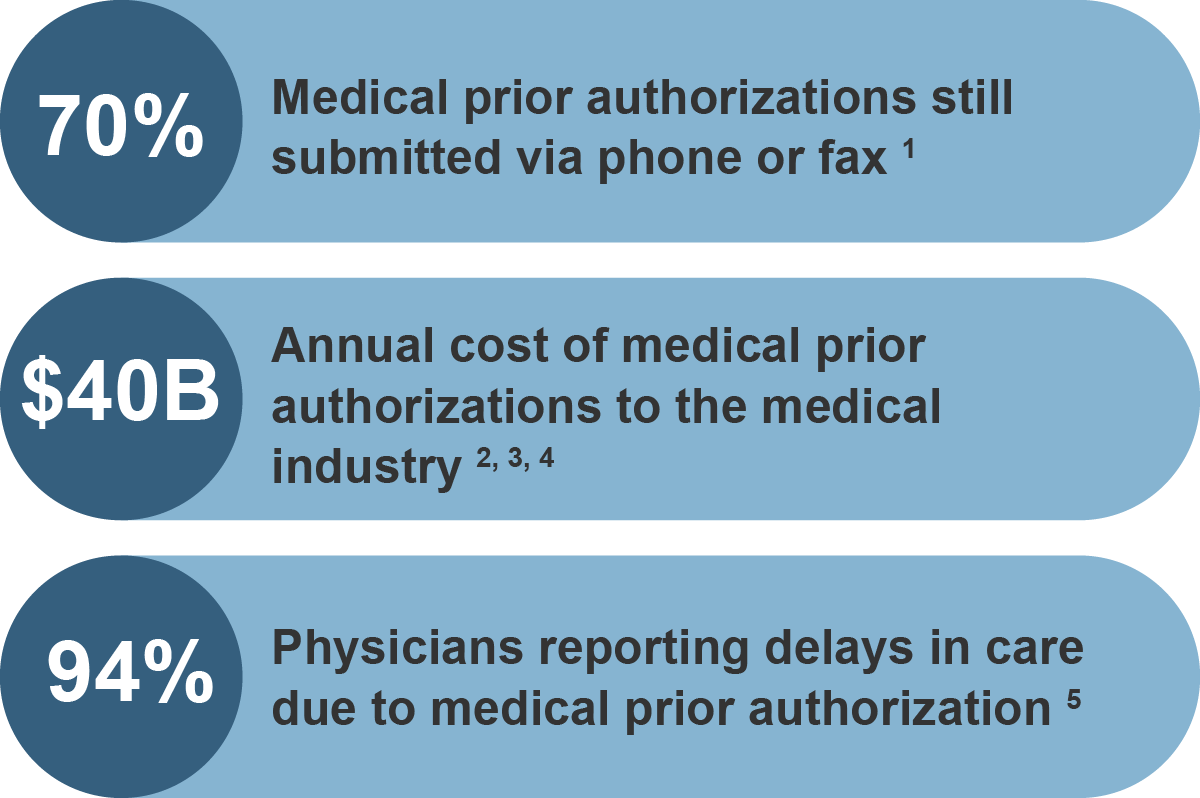

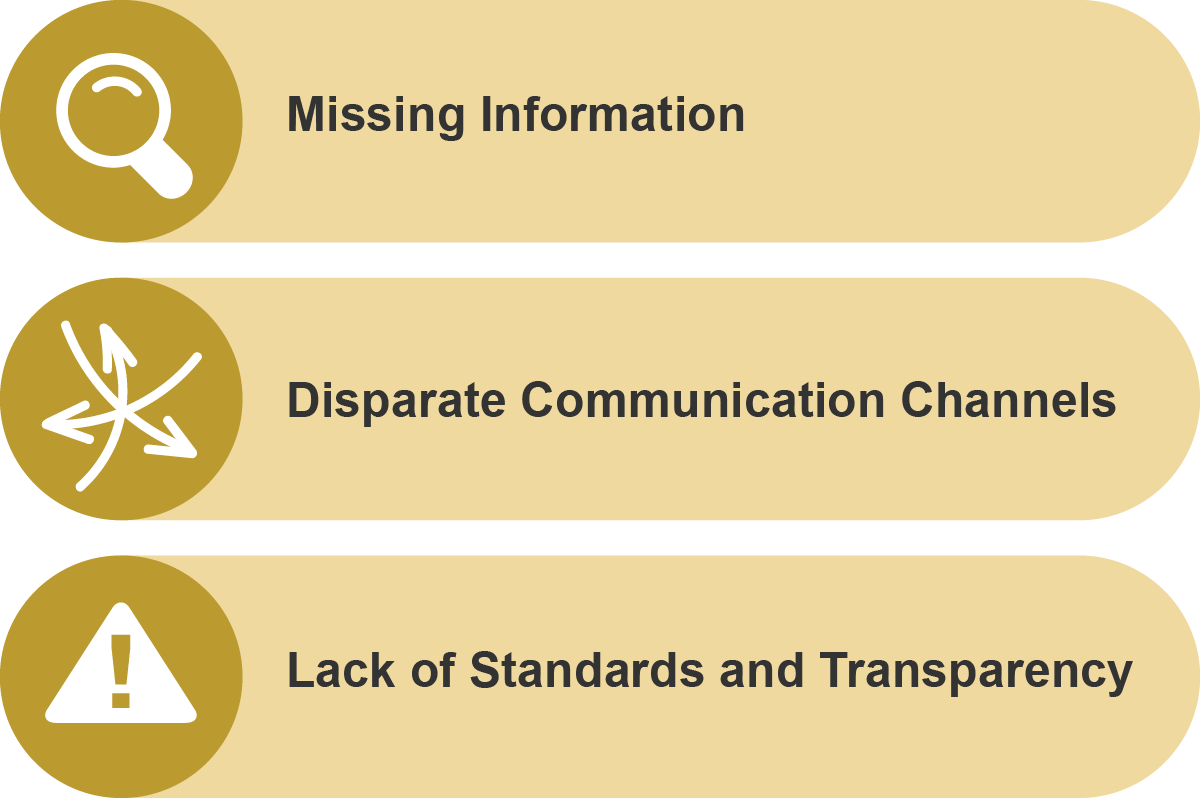
Why has it been so hard to reduce the administrative burden of PA?
Managing healthcare is complicated: the diverse parts of a health plan must work together seamlessly to deliver timely, high quality care for members and beneficiaries. A member’s demographics, their plan information, their eligibility, and their provider’s information all come together to allow the right decisions to be made at the right time by the right staff member.
Ideally, all of this information would be easily shared between providers, health plans, members, medical equipment suppliers, and other healthcare vendors. We know that currently this is not the case. The resulting cases with missing, incorrect, or invalid information slow down the entire process, delaying care for members.
Mesh captures everything you need to
make a decision, and nothing you don’t.
Mesh integrates with your existing software to automate prior authorization behind the scenes, providing a bridge to the digital transformation of prior auth—a standard way for payers to exchange information with providers about member care. Let Mesh handle the mundane administrative tasks and stop chasing loose ends in medical prior auth.

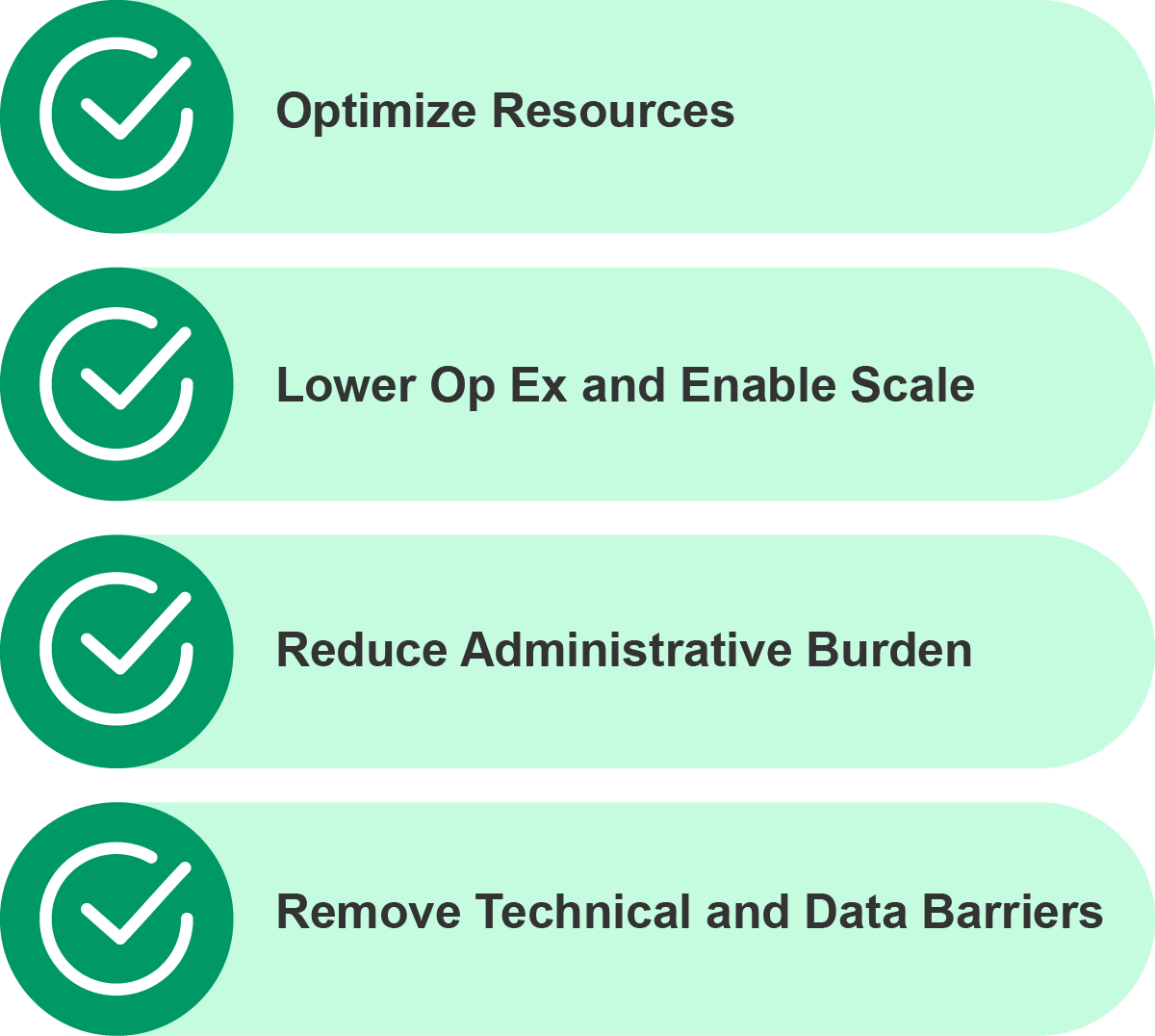
Mesh helps everyone.
From payer to providers and patients, everyone benefits from faster, accurate health care decisions. By optimizing workflows and streamlining administrative tasks, Mesh helps reduce operating expenses, and yes, it scales. Perhaps even more importantly, Mesh aids in mitigating physician burnout by fostering a more focused and patient-centric environment.

Mesh is on FHIR!
Mesh’s Smart on FHIR app allows health plans to interface with provider EHRs, seamlessly integrating clinical data with your prior auth workflow.
Mesh is also in the advanced stages of testing the proposed PARDD APIs and combining them with Mesh’s own process optimization capabilities. Let’s get the PARDD started!

Don’t Rip and Replace!
Infrastructure is a major investment, and at Mesh we understand that updating your systems can’t always mean replacing them. It’s why we operate in collaboration with your existing systems and platforms, taking in data from any source and filtering what’s most important. Mesh works behind the scenes to automate PA so your teams can focus on the most critical information at hand.
Mesh Offers

- American Medical Association. (2022). AMA prior authorization (PA) physician survey.
- CAQH. (2022). 2021 CAQH Index. Https://Www.Caqh.Org/Sites/Default/Files/Explorations/Index/2021-Caqh-Index.Pdf
- Gee, E., & Spiro, T. (2019, April 8). Excess administrative costs burden the U.S. health care system. Center for American Progress. https://www.americanprogress.org/article/excess-administrative-costs-burden-u-s-health-care-system/
- Institute of Medicine (US) Committee on Utilization Management by Third Parties, Gray, B. H., & Field, M. J. (1989, January 1). Utilization management: Introduction and definitions. NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK234995/
- American Medical Association. (2022). AMA prior authorization (PA) physician survey.
