Automating the PA steps
that don’t need people.
Accelerating those that do.
Bridging the Medical Prior Auth Divide
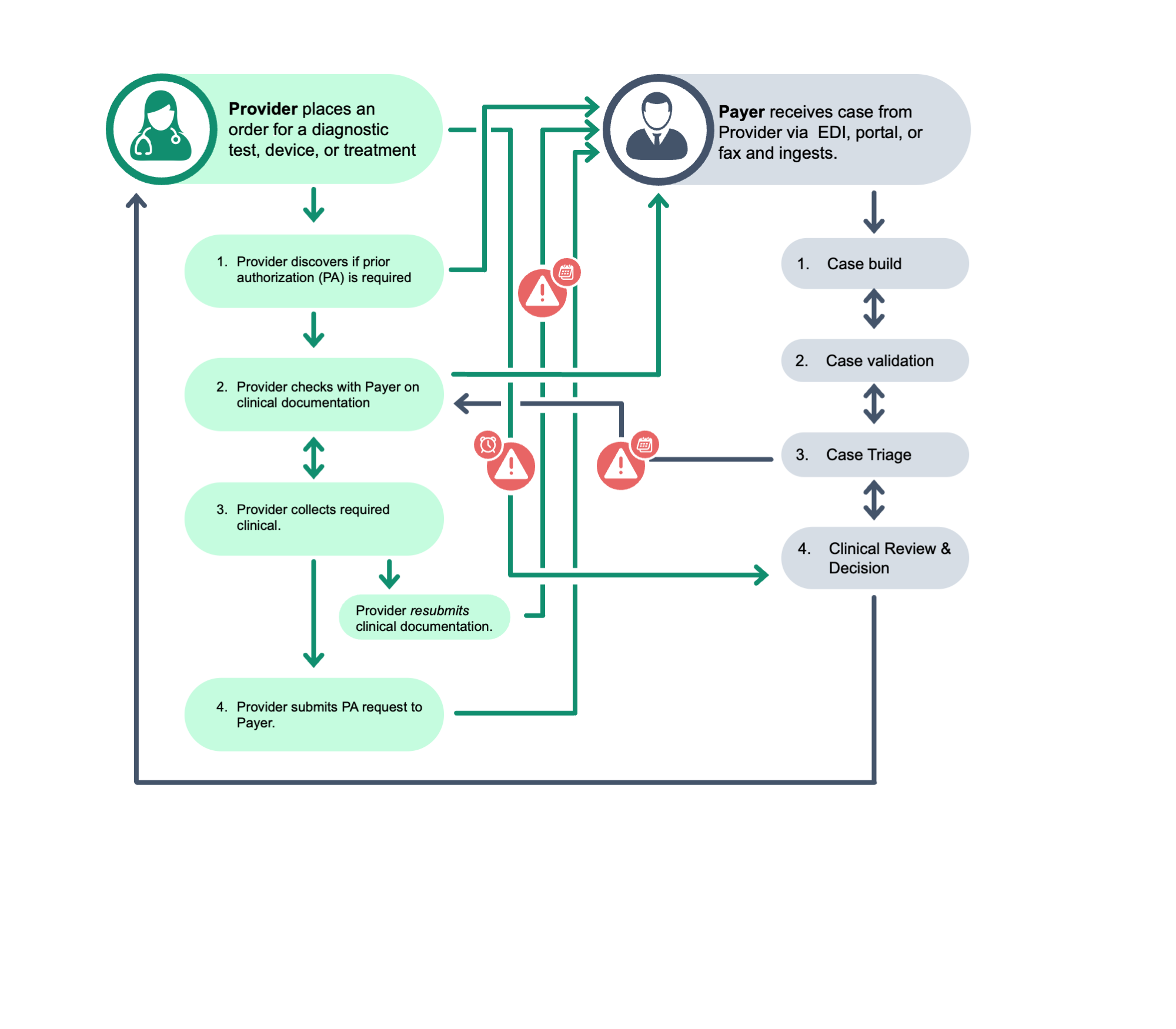
Healthcare providers and payers are increasingly turning to advanced technologies, like artificial intelligence and machine learning, to automate and accelerate medical prior authorization (mPA). But mPA is still a very manual process, and any company that claims 100% automation isn’t giving the full story. Where other companies over-promise and under-deliver on the application of technology, Mesh uses them selectively and intentionally to automate repetitive tasks that truly don’t need a human touch and to facilitate more efficient communication between healthcare providers and payers. Mesh’s technology brings critical data to the surface, ensuring the human-in-the-loop has all the information at their fingertips to work in the best interest of the patient. As we all work toward that fully automated future, there’s a lot that can be done now, and Mesh will be there, every step of the way.
Enhancing Productivity for Payers and Providers
Mesh offers payer-specific, provider-specific, and full end-to-end solutions to reduce the administrative burden medical prior auth on your teams. Each solution can be tailored to fit your organizations unique needs.
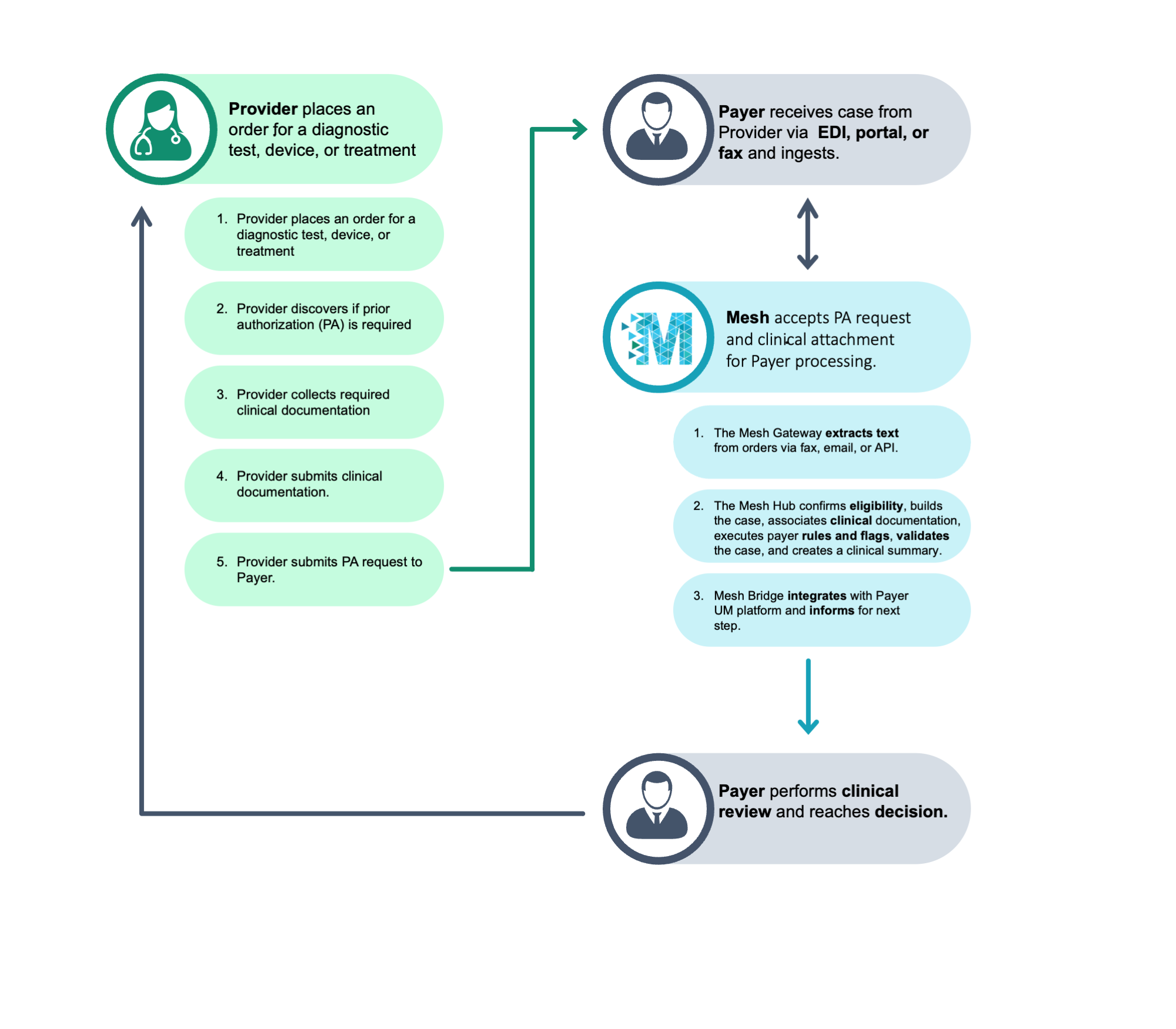
Payers

Mesh helps payers optimize intake and triage, support auto approval, accelerate clinical reviews, and reduce time to decision.
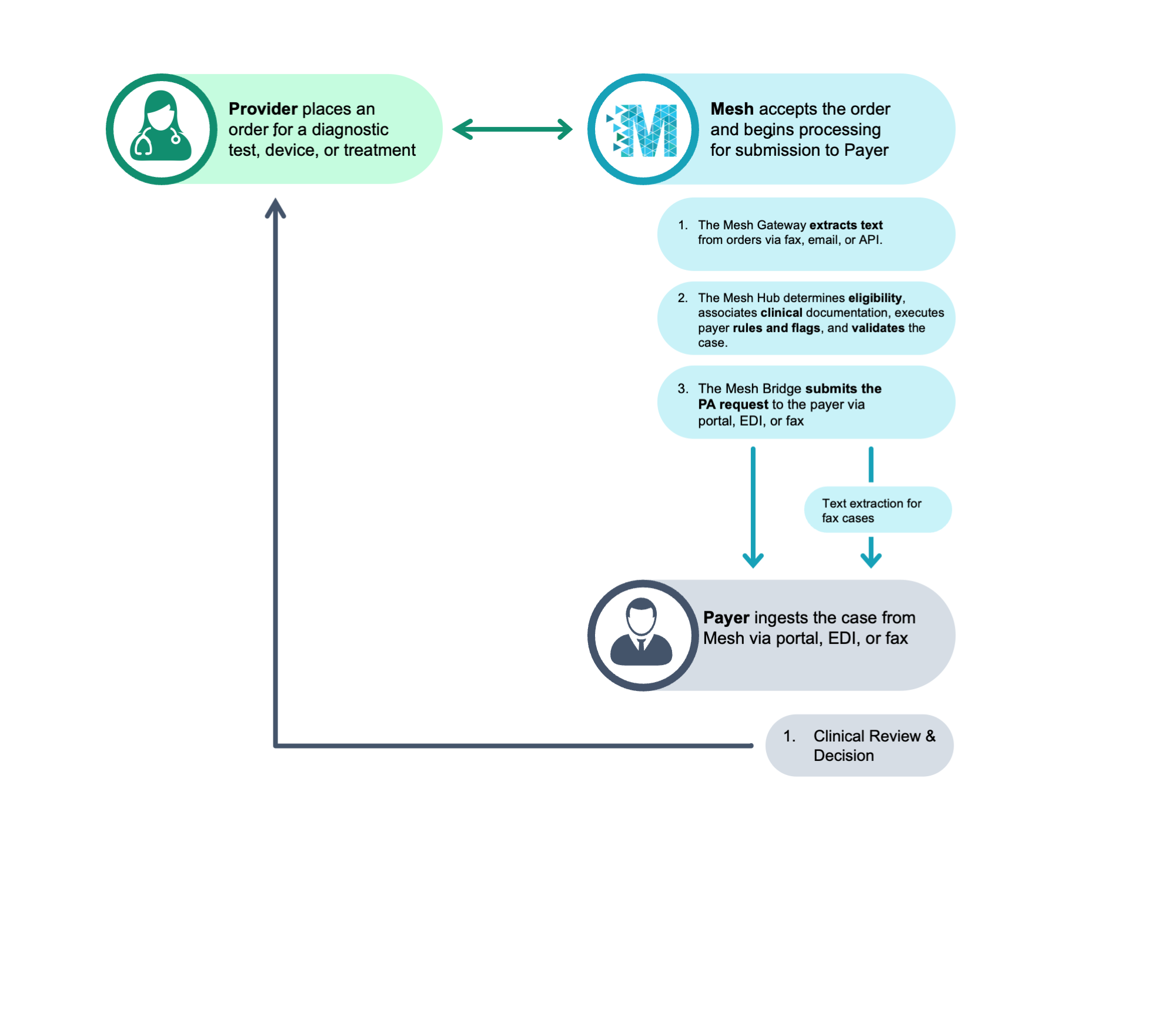
Providers

Mesh helps providers and suppliers get the transparency they need to submit appropriate information at initial request and drive to patient access.
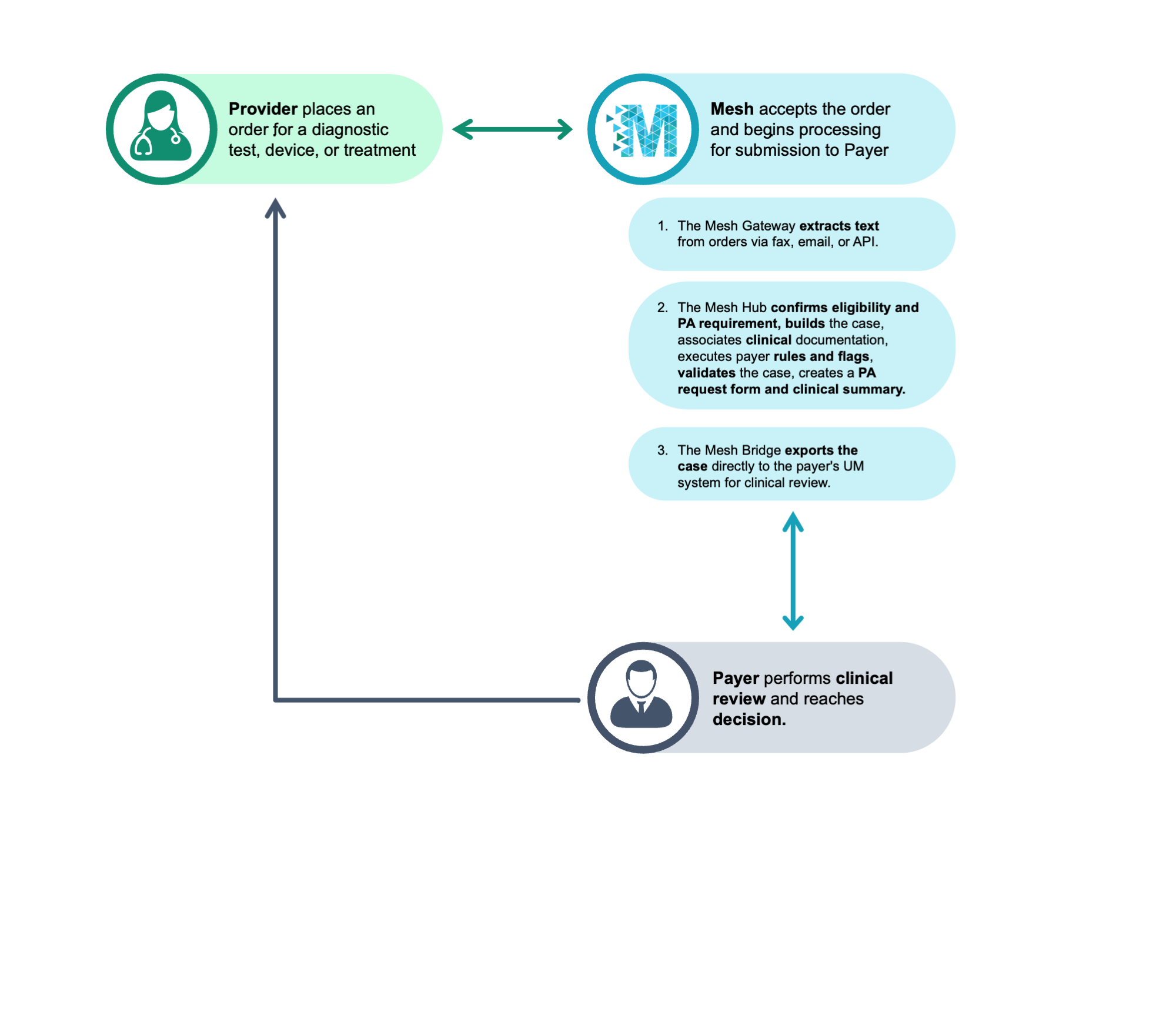
End-to-End
Mesh helps strategic payer / provider partnerships streamline mPA, from initial request to final decision.
Mesh Solution Workflows
Workflows